Nov 29, 2017
Rural Unintentional Injuries: They're Not Accidents – They're Preventable
Hot and thirsty from playing outside, a small child grabs the sports drink bottle in the garage and dies from drinking the deadly chemical the bottle contained. Grandma trips on her throw rug, the fall causes injuries so significant she eventually requires hospice care. A speeding car full of college students strikes a bridge head on, driver with phone in hand, the last text seconds before impact reading "LOL." Not one seatbelt in use, all are dead at scene. These descriptions are harsh. Tragic. Real. Sometimes friends, families, and neighbors never stop grieving for those lives lost.
Fifty years ago, these occurrences were referred to as accidents – events that were "inevitable, random, and unavoidable." But with advancements in the science of injury, the Centers for Disease Control and Prevention's (CDC) public health experts know these events are preventable. Now replacing the word "accident" with the phrase "unintentional injuries," the experts also understand that prevention depends on changing the public attitudes and behaviors that impact injury and fatality rates.
Rural Unintentional Injuries: The Deadly Causes
 Specific metropolitan and
nonmetropolitan unintentional injury
data can be found in the CDC's Web-based Injury
Statistics Query and Reporting System (WISQARS), an
"online database that provides fatal and
nonfatal injury, violent death, and cost of injury data
from a variety of trusted sources."
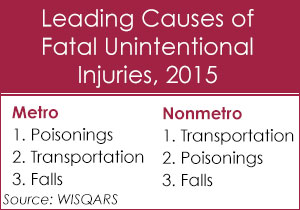
Reviewing the 2015 data, the top three categories
of fatal unintentional injuries are the same for rural
and urban areas. However, there is a notable difference
in ranking. For urban areas, poisonings, transportation
injuries, and falls rank greatest to least. But for rural
areas, motor vehicle-related injuries push poisonings to
second, with falls also ranking third.
Specific metropolitan and
nonmetropolitan unintentional injury
data can be found in the CDC's Web-based Injury
Statistics Query and Reporting System (WISQARS), an
"online database that provides fatal and
nonfatal injury, violent death, and cost of injury data
from a variety of trusted sources."
Reviewing the 2015 data, the top three categories
of fatal unintentional injuries are the same for rural
and urban areas. However, there is a notable difference
in ranking. For urban areas, poisonings, transportation
injuries, and falls rank greatest to least. But for rural
areas, motor vehicle-related injuries push poisonings to
second, with falls also ranking third.
What causes fatal unintentional injuries in the nation's homes?
 Poisonings,
falls, fires and burns. Researchers at Johns Hopkins
Center for Injury Research and Policy and Bloomberg
School of Public Health
reported the prevalence rate of poisonings is 43%,
falls 34%, and fires and burns both at 9%.
Poisonings,
falls, fires and burns. Researchers at Johns Hopkins
Center for Injury Research and Policy and Bloomberg
School of Public Health
reported the prevalence rate of poisonings is 43%,
falls 34%, and fires and burns both at 9%.
Looking at 2000-2008 data, the researchers also pointed out another concern regarding these unintentional injury death rates: residents 80 plus years of age "had the highest death rates by an enormous margin." According to the authors, "many of these deaths are due to falls."
Whether a home is rural or urban, the Hopkins researchers shared 29 evidenced-based prevention strategies geared to decreasing home injury rates and fatalities.
A recent CDC MMWR Rural Health Series report
reviewed 5 rural categories of potentially preventable
deaths. The categories included heart disease, stroke,
chronic lower
respiratory disease and cancer. In the 5th
category – unintentional injuries – a significant
disparity is highlighted: the rural death rate is 50%
greater than the urban rate. The report goes on to
suggest that the number one cause contributing to this
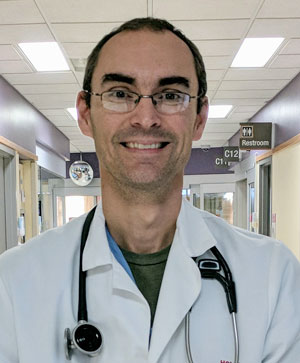
disparity is motor vehicle trauma. Dr. Richard Sidwell, a
Des Moines, Iowa, trauma surgeon and chair of the
American College of Surgeons Rural Trauma Subcommittee,
said no database makes those rural motor vehicle trauma
statistics look better.
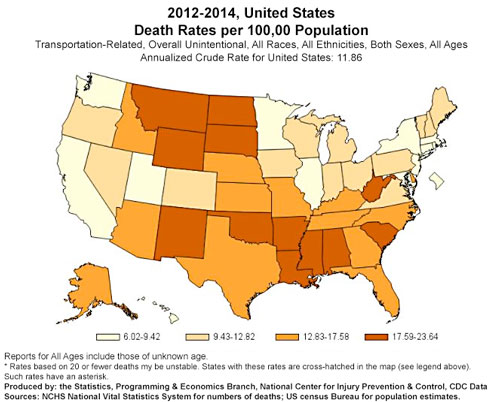
"No matter how you look at the statistics regarding rural trauma, whether it's excess deaths, likelihood of dying, preventable mortality, it's basically 50% higher when compared to urban injury," Sidwell said. "If you are injured in a rural environment with the same injury as in an urban area, you are at least 50% more likely to die. This is a consistent finding."
If you are injured in a rural environment with the same injury as in an urban area, you are at least 50% more likely to die. This is a consistent finding.

The CDC report further outlines several rural factors contributing to these traffic-related death rates. Foremost is distance, a factor compounded by two components: the distance EMS travels to a crash site and the distance from the crash site to the nearest rural medical facility. Another factor is medical expertise. With treatment at centers dedicated to trauma care, expertise that can't realistically be duplicated at the rural level, the report noted life threatening trauma is "associated with 25% lower mortality."
But despite the barriers of distance and expertise, Sidwell, who has passion for rural trauma care, said he also looks at the mortality rates in terms of delays.
"I have no doubt that delays in getting rural residents to definitive care is critically important," Sidwell said. "Some delays are outside a hospital, like the delays in discovery, summoning help or mobilizing a rural volunteer crew. Other delays occur in the rural hospital, like recognizing severe injury, or taking time trying to determine the complete extent of injuries. I believe that in the global picture, a main reason there is excess mortality in rural areas, is related to delays in getting the injured person to definitive care."
In April, the National Highway Traffic Safety Administration released Rural/Urban Comparison of Traffic Fatalities.
The good news
- Between 2006 and 2015:
- Rural traffic fatalities decreased 28%
- Rural alcohol-impaired driving fatalities decreased 34%
- In 2015, rural daytime observed seat belt use reached slightly greater than 85%, similar to urban use
The bad news
- The rural fatality rate was 2.6x higher than urban
- 28% of fatalities were associated with speeding (vs. 27% urban)
- Of rural driver fatalities, 61% are categorized as "death at scene," compared to 33% urban
- Rural vehicle occupant fatalities:
- 50% were unrestrained
- 61% of pickup truck occupants were unrestrained
Another Rural Killer: Falls. Yes, Falls Kill.
Falls, a common cause of death in both rural and urban areas, are an unintentional injury that intersects with trauma, since even ground level falls (GLFs) are traumatic events that can result in multiple injuries requiring specialty surgical care. In the aging population, experts say that GLFs are often "sentinel events" that makes obvious this population's frailty, a condition contributing to death rates. Some GLFs even have death rates near 50%, especially those associated with significant head injuries, like brain bleeds.
Table 1. 2015 Fall Fatalities
| Metro | Nonmetro | Metro/Nonmetro | |||
| Age | Total | Crude Rate* | Total | Crude Rate* | % Difference |
| 85+ | 13,154 | 251.04 | 2574 | 245.77 | 2.1 |
| 65-84 | 10,403 | 30.46 | 2356 | 32.16 | 5.4 |
| 45-64 | 3156 | 4.41 | 646 | 5.14 | 15.3 |
| 25-44 | 681 | 0.92 | 135 | 1.27 | 32.0 |
| 13-24 | 186 | 0.41 | 38 | 0.52 | 23.7 |
| 0-12 | This age group: numbers too small for accuracy | ||||
*Crude rate calculated per 100,000 population
Source: CDC's WISQARS database
But death rates in younger rural residents are also concerning. According to the 2015 WISQARS data, rural fall fatality rates further the theme of higher death rates compared to urban counterparts, specifically in age groups 13 to 64. (See Table 1.)

Dr. Mindy Renfro, a University of Montana geriatric physical therapist who's been a member of the CDC's and the National Council on Aging's work groups addressing falls, points out that there are many theories linked to differences between urban and rural fall fatality rates.
"Falls in our rural areas begin to increase around age 40," Renfro said, reviewing three theories. "First, some theories link increased falls with increased outdoor activity, ranch work, and the work on homes in rural areas where owners must do the repairs themselves, repairs often involving ladders. Another theory is that the snow belt location of many rural states also leads to an increased fall risk from ice. Lastly, people living in rural areas are often highly independent and don't ask for help as their bodies begin to change. But the bottom line? We simply don't know yet what drives the increased fall risk."
I will pose this question to patients: 'If you fall, how long will it be until someone finds you?' Because that's where the life and death part usually comes in.
Renfro, like Sidwell, points to the impact of delay from time of fall to definitive help. Renfro said when she talks with patients, students or public audiences, she uses a specific comment to highlight just how devastating falls can be.
"I will pose this question to patients: 'If you fall, how long will it be until someone finds you?'" Renfro said. "Because that's where the life and death part usually comes in."
Nationwide Fatal Unintentional Injuries Associated With Occupations Often Found In Rural Areas
- Agriculture: Transportation incidents
- Construction: Falls, struck by object, electrocution, and caught-in/between incidents comprise the "Fatal Four"
- Mining: Machinery accidents, powered haulage
- Manufacturing: Contact with object/equipment, falls
Not To Be Underestimated: Non-drug Poisonings
Sandwiched between motor vehicle fatalities and fall deaths are rural deaths from poisonings. For both rural and urban areas, the leading cause of unintentional deaths from poisonings is overwhelmingly drugs of abuse, and specifically opioids. But a look into the non-drug poisoning data is also important. Emergency medicine physician and toxicologist, Dr. Travis Olives, who practices with the Minnesota Poison Control System based in Hennepin County Medical Center, Minneapolis, is no stranger to rural fatal toxic exposures since he previously practiced emergency medicine in a Wisconsin Critical Access Hospital. Olives said the most common non-drug poisoning calls to their system from rural areas fall into several main categories.
"At the top are the alcohols that are not intended for human consumption," Olives said. "Then comes the fumes, gases, vapors that occur in the industrial, manufacturing and farm context. Common things are common, and here is where carbon monoxide is a year-long problem, especially because it's an imitator of a whole lot of other serious health conditions. Another source of toxins come from the closet of multigenerational bottles of 'stuff.' Items that grandpa and grandma, mom and dad, and now son and daughter have all left on the shelf. This mix of old cleaners and other potential poisons lies in wait for little hands that might accidentally be exposed to them."
Olives said "needless and preventable" exposures also happen because of the tendency to keep toxic liquids in containers that normally contain safe liquids.
"Coffee cups and sports drink bottles always seem to be a handy place to store toxic stuff when you're working in places like the garage," Olives said. "Handy until an adult or child drinks from it."
Preventing Poisoning Deaths: Early Intervention Is Key
The Health Resources and Services Agency, HRSA, reminds the public that the "best way to prevent poisoning is to learn and talk about" poisoning risks before an emergency. The agency provides partial support for the nation's 55 poison control centers, an integral part of the public health system and especially important to rural areas. These centers, staffed by specially trained nurses, pharmacists and doctors like Olives, are available 24 hours a day, providing free and confidential assistance. Olives said that he wants the public to understand – and especially the rural public who face the resource limitations and distance issues he knows so well – that an immediate call to the 1-800-222-1222 poison control center number can make the difference between living and dying from a drug or non-drug poisoning.
"The big theme worth hitting on over and over again is making that call and getting that early advice to answer the question: 'I think I have a problem, how big of a problem is it?" Olives said. "It's of huge importance when it comes to limited access and large geographical areas. We can do a lot of good by helping someone with that question, whether it's a medic in a rig, a parent at home, or a doc in a small hospital who wonders if they should transfer or keep a patient. We can help with those questions early, long before any other management needs to happen to get the ball rolling. Or we can put the brakes on if it's not as big a deal as people think."
The big theme worth hitting on over and over again is making that call and getting that early advice to answer the question: 'I think I have a problem, how big of a problem is it?
Olives acknowledges that this coordinated work is one of the reasons their poison control center calls itself a "system." He also hopes that "system" also helps bring awareness to the wider expertise they provide other than childhood ingestions.
"We cover all ages, and all periods of life," he said. "We see a variety of substances and exposures, everything from street drugs that are smoked or injected or snorted, to chemical exposures at factories and on farms, to questions about the possibilities of poisonings associated with food. We serve people across the spectrum of life, across a huge spectrum of poisonings."
The Panic with a Poisoning: How Poison Control Centers Can Help
Those who best understand the value of the nation's poison control centers are those who used a center for a life-threatening poisoning event. This video shows how the Minnesota's Poison Control System brought "system" care to a rural family and hospital:
Back To Falls: Prevention Strategies
For a comprehensive and unified fall prevention effort, advocacy groups, such as the National Council on Aging, and members of the American Physical Therapy Association (APTA) and the American Occupational Therapy Association (AOTA), join up with federal prevention programs, like the CDC's STEADI program.
Renfro said fall prevention strategies require forethought, time and planning, but the most important prevention strategy is actually having the frank conversation about fall prevention in the first place.
"Falls can either change a life forever, or actually be the cause of death. And they are not a normal part of aging," Renfro said. "For some geriatric patients, a new medication may make them unsteady. For others, their glasses aren't correct and depth perception is a problem. Sometimes, a patient's balance has been affected by another condition, like a stroke."
To emphasize one of the most important aspects of fall prevention – the gap between giving prevention advice and having that advice implemented – Renfro said she uses a humorous example from her own family to teach audiences and students.
"When I'd go home to visit my mother, I'd get rid of all of her throw rugs, warning that they are a prime cause of falls," Renfro shares. "Every year I'd come back, there'd be more rugs. When my mother turned 90, I finally asked her 'what's the deal?' She told me every time I threw her rugs out, it gave her the opportunity to redecorate with new ones."
Renfro shares this personal story as a good example of how people might smile, head nod, assure you they're serious about eliminating their fall risks, but then not make any changes at all.
"You've got to address people's reality," she said. "So, now, my mother still refuses to give up her throw rugs, but she does agree to getting rugs with ramped edges. We make sure they're secured on the floor and she does heel stretch exercises to make sure she has adequate "toe lift" up and over the rug edge, a poor lift being the result of too many years in high heels."
Reducing Rural Motor Vehicle Fatalities: Educating Healthcare Facilities and The Public
Poisonings and falls, number two and three on the WISQARS 2015 rural fatality list, are important public health issues. But, it's that rural motor vehicle fatality and disparity rate that owns what might be the most sobering of all unintentional injury statistics: the 50% difference in fatality rates compared to urban. Though many factors impact fatality rates, trauma surgeon Sidwell said that decreasing the time to definitive care after a patient reaches a rural hospital could help make a difference. How can that time interval be shortened? Sidwell said it starts with training efforts.
Reviewing important history, Sidwell said the popular-and-sometimes-mandated Advanced Trauma Life Support (ATLS) education course actually had rural beginnings in the 1970s due to the efforts of an orthopedic physician. The orthopedist's family tragedy involving an airplane crash in a cornfield prompted him to recognize that rural trauma care was a "system, not a doctor" problem. He and several colleagues then developed ATLS for rural providers so they'd have the training needed to provide basic care to the severely injured patients not often seen.
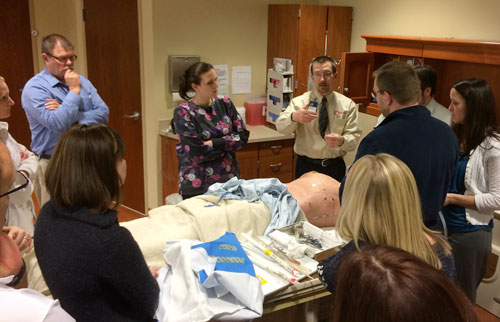
"The ATLS course was so successful, it soon became geared to trauma care in metropolitan areas," Sidwell said. "So in the late 1990s, several of our rural surgeons wanted to bring that training back to our rural providers. They created what is now the 'Rural Trauma Team Development Course.'"
The Rural Trauma Team Development Course (RTTDC) "emphasizes a team approach to the initial evaluation and resuscitation of the trauma patient at a rural facility." The course (no longer available online), its 4th edition completed in 2016, has been gaining traction, building evidence for its effectiveness (no longer available online). As of 2011, it's an official American College of Surgeons' educational program, offering Continuing Medical Education (CME) units.
Sidwell, an author on the most recent update, said the course is taught by trauma surgeons and most often is used in two ways: as part of an urban trauma center's outreach; or as part of an individual state's rural health infrastructure. Some states, such as Arkansas, use state health department funding to provide courses in their state. In 2016, the RTTDC reached 3,000 participants through 175 course presentations. Sidwell said the course not only brings knowledge, it builds relationships.
"When the urban team giving the course actually sees a small facility, they better understand the realities it faces, especially the resource limitations," Sidwell said. "And when you better understand it, you can build a relationship with the providers that work there."
 Unintentional motor vehicle injuries are
considered one of the CDC's seven
"winnable battles."
Several of their evidence-based prevention strategies
are of note:
Unintentional motor vehicle injuries are
considered one of the CDC's seven
"winnable battles."
Several of their evidence-based prevention strategies
are of note:
For alcohol-impairment:
- Check points
- Zero tolerance laws
- DUI interlocks
For restraints:
- Primary seat belt laws (independent seat belt violation ticketing, as opposed to a secondary law which allows seat belt violation citation if another offense committed)
- Child safety seat laws
Sidwell also points out that being on a trauma team
doesn't end with bringing education to healthcare
providers. It also means bringing education to the
public. Trauma surgeons are often involved with multiple
public health preventive efforts, such as helmet laws or
distracted driving prevention. He said he also believes
in public health initiatives like the recent National
Academies' Health and Medicine Division's conversation on
"getting
to zero," a plan integrating military and
civilian trauma systems. Additionally, a September
CDC MMWR report looked at seat belts in relationship
to rural fatalities. That report also highlighted the
National Safety Council's and U.S. Department of
Transportation's October 2016 launch of
Road to Zero initiative, an initiative with a goal to
eliminate road traffic deaths in the United States within
30 years.
"But to get to zero," Sidwell said, "we're going to have to specifically address the rural trauma death disparity numbers and how we're going to make a difference."
Other Unintentional Injury Prevention Resources
Falls
- National Council On Aging
Poisonings
- Health Resources & Services Administration (HRSA)
Motor Vehicle Accidents
- AAA Foundation For Traffic Safety
- Centers for Disease Control and Prevention
- U.S. Department of Transportation

