May 24, 2023
When It's Not Enough: Sleep's Impact on Rural America's Health and Safety
 Not only providing a clue to overall
well-being, the question seems a universal cultural
nicety: "How'd you sleep?"
Not only providing a clue to overall
well-being, the question seems a universal cultural
nicety: "How'd you sleep?"
Experts acknowledged that a recent surge of interest about sleep — likely due to best-selling books, sleep infomercials, and wearable sleep technology — is spotlighting links between sleep and its impact on health and public safety. Primary care and sleep medicine providers joined public health researchers and state Extension leaders to provide insight into the nuances of sleep in rural America.
From the Frontlines: Rural Residents and Sleep Concerns
Jennifer Brull, MD, an American Academy of Family Physicians board of directors member who is just stepping away from 20 years of practicing family medicine in Plainville, Kansas, said sleep concerns were a common primary complaint in her practice.

"At least once or twice a week, I'd have folks who'd show up and say, 'I can't sleep!' as their primary complaint," she said, adding that the concern was a frequent presenting symptom in all age groups. "They'd tell me that 'I'm tired all day,' or 'I fall asleep in the middle of the afternoon.'"
Brull also said that although sleep problems presented as a primary concern, they presented in a less obvious but also impactful manner.
"Sleep also shows up as 'incident to' other presenting complaints," she said. "For example, when you're working with a patient on addressing blood pressure that's too high, or diabetes that's poorly controlled, or mental health conditions like depression and anxiety, a sudden change in the stability of chronic conditions is often linked to sleep patterns."
Rural America's Sleep Patterns
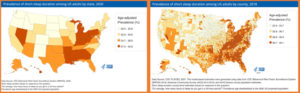
A 2022 Centers for Disease Control and Prevention (CDC) data brief included information on trouble falling asleep and staying asleep by sociodemographic and geographic characteristics. Federal surveys focusing on sleep have also provided county- and state-level results and within the category of health risk behaviors, more local data can be found on the CDC data website, PLACES.
Sleep and Rural Mental Health
Endorsing Brull's observation that the "incident to" sleep issues can be closely linked to behavioral health conditions, mental health clinicians emphasized that, along with diet and exercise, sleep is one of the three health behaviors key to mental health.

Having lived in both rural Wyoming and North Dakota, board-certified clinical psychologist Tess M. Kilwein, PhD, operates a teletherapy practice with 75% of their patients located in the rural areas of 4 states.
"I don't know that I've ever cared for a patient that hasn't had a sleep issue," Kilwein said. "Sleep disruption is characteristic of just about every known mental health diagnosis."
Pointing out that the stigma around mental health issues still remains high on the list of rural barriers to seeking behavioral healthcare, Kilwein suggested that sleep questions are helpful in gaining insight into patients' mental well-being.
"For example, before deciding on a referral to behavioral health, asking a question about sleep is crucial," they said. "It's a compassionate, non-judgmental approach to discussing sensitive topics like substance use and mental health."

Lois Krahn, MD, psychiatrist, sleep medicine specialist, and medical educator, shared an additional rural perspective on sleep deprivation's impact on mental health.
"Some people who are perceived as unpleasant to be around, or really unhappy, irritable, reactive, and just overall miserable, are actually horrendously sleep-deprived," Krahn pointed out, adding that sometimes there's even a concern that a personality disorder exists.
"However, if someone is in the middle of grain harvest, or working during commercial fishing's limited seasonal hours, or doing shift work in a rural manufacturing business or in healthcare — or even living with an undiagnosed sleep disorder — they might be getting only three hours of sleep when they should be getting at least seven," she said. "Whatever the situation, mood can be affected. Often, and even with only small interventions, their sleep can be so dramatically improved those who have been so unpleasant become calmer and kinder."
The Language of Sleep
 Experts
pointed out that doctors and researchers talk about
insufficient sleep, sleep deficiency, and sleep
deprivation all being caused by sleep disorders and
sleep hygiene practices. Sleep
deprivation is the condition caused by not enough
sleep. Sleep
disorders have multiple causes, ranging from those
linked to airway problems to others linked to
identifiable disruptions in the brain's sleep control
centers. Sleep
hygiene — not to be confused with how dirty a
sleeping area is — refers to personal habits and
behaviors linked to going to bed and getting up. More
detail on sleep can be found in the National Heart,
Lung, and Blood Institute's plain language brochure,
Your Guide to Healthy Sleep.
Experts
pointed out that doctors and researchers talk about
insufficient sleep, sleep deficiency, and sleep
deprivation all being caused by sleep disorders and
sleep hygiene practices. Sleep
deprivation is the condition caused by not enough
sleep. Sleep
disorders have multiple causes, ranging from those
linked to airway problems to others linked to
identifiable disruptions in the brain's sleep control
centers. Sleep
hygiene — not to be confused with how dirty a
sleeping area is — refers to personal habits and
behaviors linked to going to bed and getting up. More
detail on sleep can be found in the National Heart,
Lung, and Blood Institute's plain language brochure,
Your Guide to Healthy Sleep.
More on Rural America's Sleep Patterns
In addition to sleep's impact on mental health, experts said that research is clearly linking sleep deprivation to physical health: for example, the increased risk of getting type 2 diabetes, becoming obese, difficulties with weight loss efforts, and even worsening dementia symptoms. There is also some evidence that lack of sleep is possibly linked to certain cancers, their incidence, treatment outcomes, and survivorship.
Brull shared more about the sleep problems that commonly presented to her office.
"You would think if somebody needed more sleep, it'd be the folks who have more miles on them," Brull said. "In my practice, it was actually the teenagers. They'd tell me that their late nights were often due to watching online videos. Long travel time to away sports events was another situation. So, when I talked to teens and their parents, I talked about the goal to get at least nine hours of sleep every night to be able to function in a way that is healthiest for their bodies and brain."
She said that her advice of starting with designating their morning wakeup time and counting back to determine their bedtime "seemed to 'blow them away!'"
"They'd say, 'What? Nine o'clock? That's just when my social hour gets started!'" Brull said, pointing out that in addition to watching videos, teens often spend late evening hours interacting with friends on social media platforms. "It's interesting to see them start doing the math around those figures, thinking, 'I need nine hours of sleep and I have to get up at six?' and say, 'How is that gonna happen?'"
Brull added that when those calculations reveal an accumulating sleep deficit, "I'd wind up talking about 'catch-up sleep.'"
Sleep Debt
 Researchers suggested that sleep intervals that
are too short can lead to a
sleep debt. If an individual's sleep need is 8
hours/day but they only get 6, the sleep debt is 2
hours. If that pattern happens for 3 days in a row, the
debt rises to 6 hours. If on the fourth day, the
individual wants to pay back that slept debt,
it doesn't need to be paid back hour for hour. Instead,
research shows that after a sleep debt builds, a deeper
rest happens with subsequent longer sleep duration.
Although the exact number of sleep hours required to
eliminate a debt is unable to be calculated, experts
said additional sleep definitely helps pay down the
debt.
Researchers suggested that sleep intervals that
are too short can lead to a
sleep debt. If an individual's sleep need is 8
hours/day but they only get 6, the sleep debt is 2
hours. If that pattern happens for 3 days in a row, the
debt rises to 6 hours. If on the fourth day, the
individual wants to pay back that slept debt,
it doesn't need to be paid back hour for hour. Instead,
research shows that after a sleep debt builds, a deeper
rest happens with subsequent longer sleep duration.
Although the exact number of sleep hours required to
eliminate a debt is unable to be calculated, experts
said additional sleep definitely helps pay down the
debt.
Regarding teenage sleep challenges, Evin Jerkins, DO, a
rural family medicine-turned-sleep medicine provider
practicing in rural
Lancaster, Ohio, added to Brull's comments.
"It's important to understand that transitioning from childhood to adolescence involves major changes in sleep needs," Jerkins said. "Getting enough sleep is a real issue for rural teens with before- or after-school jobs or their farm chores. We're really helping our kids if we understand their sleep needs better."
More on Rural Causes of Sleepiness
In contrast to Brull's family medicine practice that sees many teens with sleep concerns, Jerkins said in his rural sleep medicine practice, he most frequently evaluates seniors, finding that social isolation is often a factor for their sleep health.

"Some seniors actually have long-standing and undiagnosed sleep disorders, so having a sleep lab here in our area is incredibly important for those diagnostics," he said. "However, during an evaluation, I often discover that many seniors are simply falling asleep because they're bored, or because they have no social interaction. If they live an hour out on a country road, there are no local activities to attend. So, I find out when they're most likely to fall asleep, and together we figure out a practical activity to slot into that time, like calling friends and family."
Brull also detailed several generalities around the patterns of insufficient sleep seen in adults. For example, painful medical conditions like arthritis might keep someone awake. On the flip side, sedating medications taken for heart conditions may also disrupt a sleep cycle, causing either sleep or dozing during the usual awake hours, a pattern that affects bedtime sleep. She also emphasized that these situations might stand alone or even be more complex if sleep disorders — either diagnosed or undiagnosed — are in play, like obstructive sleep apnea (OSA) or restless legs syndrome with its uncontrollable movements.
Heart Health and Sleep Health

Jerkins, a member of the American Academy of Sleep Medicine (AASM), also described another consultation pattern he sees in the five-county area his organization, Fairfield Medical Center, serves in rural Ohio: The majority of his patients are either self-referred or referred from a variety of physician practices, like cardiovascular practitioners who often refer because of the well-documented link between sleep disorders and common cardiovascular problems such as heart failure, coronary artery disease, and rhythm problems such as atrial fibrillation.
As Jerkins indicates, cardiovascular diseases, a category found to rank highest in a 2017 report analyzing rural deaths, have also been found to be linked to sleep issues. In 2022, the American Heart Association (AHA) added sleep habit assessments to its recommended routine questions around diet and physical activity, with the organization updating its "Life's Essential Circle" from seven elements to eight, to now include sleep. The organization's sleep recommendations include "7-9 hours of sleep for adults and more for children depending on age."
Sleep's Impact on Rural Driving
Experts also highlighted sleep's influence on another activity of daily rural living: driving.
"In rural America, we drive everywhere to do anything," Brull said. "Everyone is on roads for long distances with a landscape that is often unchanged for long intervals. Although there are many factors that contribute to rural traffic accidents, the consequences of sleep deprivation are some of them."
Brull and Jerkins both said especially concerning for their rural populations is the impact of insufficient sleep for residents commuting long distances — and a long commute plus an afternoon or evening shift at work. Those scenarios, these clinicians said, are especially impactful on sleep intervals and become a worrisome public health concern for driving.
When I think of rural populations and sleep deprivation, the problems shift workers have with drowsy driving is one of my greatest concerns.
"When I think of rural populations and sleep deprivation, the problems shift workers have with drowsy driving is one of my greatest concerns," Jerkins said.
He said these shift workers often tell him that although they recognize they're drowsy on their commute, they're not aware that they fall asleep at the wheel, a problem that translates into a major public safety concern.
"I talk to them about being responsible for driving drowsy," Jerkins said. "I'm always telling my patients, 'Don't do it. Don't drive drowsy. You can hurt or even kill yourself. And remember: You could hurt or kill someone else. There is no substitution for sleep.'"
Anne Wheaton, PhD, is the Deputy Associate Director for Science in the Division of Population Health at the Centers for Disease Control and Prevention (CDC). She provided further comment related to sleep insufficiency and rural traffic accidents.
"We know from the National Highway Traffic Administration that drowsy-driving crashes and fatalities are more common in rural areas," she said. "It's important to recognize that drowsy driving not only occurs when a driver hasn't slept enough or has an untreated sleep disorder, but it can also be related to some over-the-counter or prescription medications."
She added more information on drowsy-driving patterns, a category most recently studied by Louisiana researchers who found that their state's patterns were also clustered in rural areas.
"What often goes unrecognized is that the drowsy driver doesn't actually have to fall asleep to have a crash," she said. "Drowsy driving makes people less able to pay attention to the road, slows their reaction time, and affects their decision-making ability, resulting in less safe choices."
Wheaton reviewed several countermeasures to driving drowsy, like the rumble strip.
"One intervention is rumble strips," she pointed out. "They're located on long stretches of rural roads with a primary purpose of serving as a physical and audible alert when a sleepy driver starts to go off the road."

Seema Khosla, MD, is a North Dakota pulmonologist and sleep medicine specialist and chair of the AASM's Public Awareness Committee. Providing sleep healthcare to people from rural North Dakota, South Dakota, and Minnesota, she said questions around rumble strips can serve as a valuable assessment tool.
"When I sense that a patient might be minimizing their sleep deprivation's impact on their driving, I'll ask them, 'Have you ever hit the rumble strips?' she said. "If they answer, 'All the time.' I immediately have a better understanding of the seriousness of their sleep condition. Even if the answer isn't 'all the time,' the question is still helpful. Once we discuss the purpose of rumble strips, they often admit to having hit them from time to time. Then comes my follow-up question: 'Do you pull off at the next exit to take a nap or call for a ride home?' While many have hit the rumble strip, very few have recognized the seriousness of this and have gotten off the road. It's a good way to begin the discussion of sleep and safety."

More on Sleep and the Rural Workplace…
In addition to the public health impact on driving, clinicians also discussed how sleep impacts public health due to its tie to many causes of rural unintentional injuries. CDC's Wheaton described how insufficient sleep ties specifically to workplace injuries.
"Aside from the drowsy-driving issues, sleepy shift workers or workers doing long shifts are faced with safety issues associated with workplace injuries," she said, adding that the CDC's National Institute for Occupational Safety and Health (NIOSH) has special online education for emergency responders (no longer available online) and nurses in these work situations.
Jerkins shared that workplace-related concerns are another common reason patients seek his consultation, often because they've had a "near miss" at work, fallen asleep at work, injured themselves — or almost injured someone else at work.
"These consultations tend to be fairly dire, often with their jobs at risk," he said, sharing that undiagnosed OSA is a common medical condition causing many sleep problems. "I tell them 'We're going to make a plan and, with your permission, we'll let your employer know we're working on this.'"
Sleep's Economic Impact: Tied to Healthcare Access for Sleep Concerns
In addition to workplace injuries, sleep deprivation impacts worker productivity. In 2017, the RAND Corporation completed a global analysis detailing overall economic impact, revealing that the U.S. ranks highest in estimated annual losses. To mitigate these economic losses, the report posed several solutions for both employers and public authorities, ranging from organizational cultural changes around recognizing sleep's multifaceted importance to support for professionals caring for the population's sleep health.
Sleep experts also suggested that support might start with bridging the gap in healthcare provider education. AASM's Khosla pointed to a 2021 study revealing that medical students get less than three hours of education on sleep. Despite sleep's impact on mental and physical health, the report also revealed that sleep education is not "a core educational requirement" for primary specialties like pediatrics, internal medicine, and family medicine. Lastly, the analysis noted that education gaps exist even in "specialties thought of as inclusive for sleep health" — neurology and pulmonology — who only receive "a few hours of didactics."
Recognizing the need for increased sleep health awareness for not only healthcare professionals but also for the lay public, AASM's Khosla emphasized that even basic messaging can be a start.
"We have good messaging that for stroke or heart attack symptoms people need to go to the ER," she said. "But for non-emergent symptoms like snoring, a common symptom of OSA, there's little awareness of how serious that condition can be," she said, adding that a goal of her organization is to increase public awareness about good sleep hygiene along with recognition of treatable sleep disorders.
Federal Support for Increasing Awareness
Khosla also pointed out that AASM is now continuing specific work around OSA with CDC funding support to "form a coalition of partners and collaborators that will work together to make a widespread and measurable effect on obstructive sleep apnea public and professional awareness."
Sleepless in Nebraska: University of Nebraska-Lincoln Extension's Sleep Education Program
As the experts pointed out, sleep education is not widely available for urban or rural populations. One of the few current public sleep health education programs is led by University of Nebraska-Lincoln (UNL) Extension. The backstory to the program starts at a 2016 meeting of the Franklin and Kearney County Extension boards.
"When I mentioned creating a sleep education program to address sleep deprivation, every single board member's head bobbed 'yes' and I took that as a go-ahead," Susan Harris said.

Harris was the area's Extension Rural Health, Wellness, and Safety educator. Between 2017 and her retirement in late 2022, Harris got the Sleepless in Nebraska program launched, collaborative research on farmers' sleep patterns completed, and multiple public presentations delivered, reaching hundreds of elementary school children, teens, and adults. The messaging also reached a national audience when, in 2020, Harris was interviewed on several occasions by USDA Radio News.
Hearing of Harris's retirement plans, Hannah Guenther, a
family consumer science teacher and UNL Foods and
Nutrition Extension team member who'd attended Harris's
presentations, recognized two things: the program was too
important to not be continued after Harris's retirement
and that she herself, as an educator and a farm wife,
recognized her own passion to provide sleep education for
Nebraskans, especially those in rural areas.

Taking on a sleep program leadership role this year, Guenther described the program as geared to all ages, to multiple occupations and life roles, and having a triple focus: sleep for health, sleep for safety — including drowsy driving education — and sleep for rest and restoration.
"We tell our audiences that it's OK if they're yawning during our presentation, because our goal is for them to walk away with several tips that will actually make them sleep better that night," Guenther said.
Two tips she finds well-received by teens and other audiences are the importance of establishing a "same time wake time" and a specific time to turn off blue light, the light spectrum associated with laptops, phones, and other electronic devices known to disrupt the brain's sleep cycle centers.
Another topic Guenther said that seems to resonate with teens is education around getting settled in for a good night's rest.
"Teens tell us one of the main reasons they can't fall asleep is because they can't slow their thoughts from jumbling around in their mind, something referred to as 'monkey mind,'" she said. "One suggestion we offer is to keep paper and pencil handy to write some of those things down. For example, just putting down the thought 'Don't forget to pack lucky socks in my basketball bag for tomorrow's game' on a list can go a long way."
Guenther said she believes that the program presentation numbers are directly related to the importance of the program. By mid-March 2023, she noted 20 presentations already scheduled. She shared her perspective on the program's outcomes.
"As an Extension team member, my goal for any education we provide is that people walk away with information they can apply to their life immediately," she said. "We want to offer easy-to-understand and easy-to to-access information. We're pleased that the immediate feedback we get indicates that people are taking seriously our recommendation that even one behavior change might make a major difference in how well they sleep. We don't want them to walk away thinking they have to completely overhaul their life. My favorite outcome is that they understand that just one thing can make a really big difference."
Resources
American Academy of Family Physicians
- Sleep Disorders in Adults
- Sleep Disorders in Children
- Assess and Improve Your Sleep
- Insomnia
- Sleep Changes in Older Adults
American Academy of Sleep Medicine
- Bedtime Sleep Calculator
- Sleep Education Information
- Sleep Team Training
- Sleep Medicine Professional Development
American Heart Association
Centers for Disease Control and Prevention
- Basics About Sleep
- Drowsy Driving: Asleep at the Wheel
- National Institute for Occupational Safety and Health (NIOSH)
National Highway Transport Safety Administration
National Road Safety Foundation
- True stories: Drowsy Driving
National Institutes of Health
- National Heart, Lung, and Blood Institute
- National Institute on Aging

