Sep 25, 2019
Effective Communication and Consistency in Increasing Rural Vaccination Rates
by Allee Mead
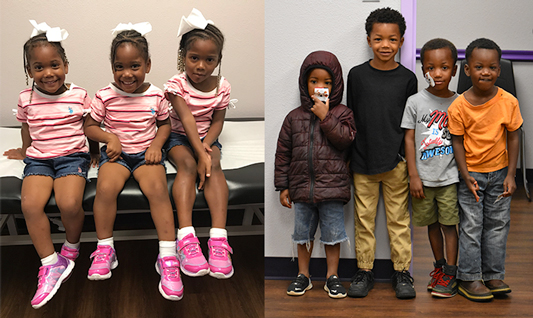
Diane* brought her four children into Pelican Pediatrics, a Rural Health Clinic (RHC) in rural Homer, Louisiana. Since Diane and her family had moved in and out of the state quite a bit, Leslie Brasher, nurse practitioner and RHC owner, met with Diane to discuss the children's medical records. Brasher discovered that only the oldest child had received any vaccines.
When Brasher asked why, Diane said that the firstborn had experienced health issues around the time of receiving the first set of infant vaccines. However, when Brasher reviewed the medical records, she discovered that the oldest child had been admitted for breathing problems at the age of one month — before the child would have received any vaccines.
“Mom's timeline was not accurate and vaccines got the blame,” Brasher said. She's currently working with Diane to get all four children up-to-date on their vaccines.
Barriers to Vaccination in Rural Areas
About 97% of Pelican Pediatrics patients are insured through Medicaid. “We are in a rural area where there is a lot of poverty. Jobs are hard to come by and many parents lack sufficient education and resources,” Brasher said. “Sometimes wellness checkups fall pretty low on families' list of priorities when there are issues like food security.”
Sometimes wellness checkups fall pretty low on families' list of priorities when there are issues like food security.
In addition to financial issues that prevent getting to a clinic appointment, other barriers to vaccination include distance from healthcare facilities and a shortage of providers. Shannon Stokley, DrPH, Associate Director for Science at the CDC's National Center for Immunization and Respiratory Diseases, said, “We're working with academic researchers to better understand: What are the challenges to vaccination in these areas, but also what are effective strategies to promote vaccination?”
According to a CDC Morbidity and Mortality Weekly Report (MMWR) article from October 2018, children younger than three years old living outside of metropolitan statistical areas (MSAs) are receiving recommended vaccines at lower rates (a difference ranging from 2.6 to 6.9 percentage points) than children in MSA principal cities. An MMWR article from August 2019 shows that non-MSA adolescents face an even greater disparity: There was a 15.4 percentage point difference between non-MSA teens and those living in MSA principal cities for receiving the human papillomavirus (HPV) vaccine series and a 19.7 percentage point difference for the second dose of meningococcal conjugate vaccine.
Navigating Vaccination Language
Glossary of vaccinations included in this article:
- HepB: hepatitis B
- DTaP: diphtheria, tetanus, and acellular pertussis (its booster shot is called Tdap)
- PCV: pneumococcal conjugate
- MMR: measles, mumps, and rubella
- VAR: varicella (also known as chicken pox)
- HPV: human papillomavirus
- MenACWY: meningococcal conjugate
The CDC provides a full list of vaccines, abbreviations, and recommended child and adolescent immunization schedule.
When it comes to vaccines required for school entry,
Stokley reported that there is little difference between
rural and urban rates. However, when it comes to vaccines
that are not required by most states — like the
HPV and meningococcal conjugate vaccines —
rural vaccination rates are lower. Stokley suggested that
rural patients and providers might prioritize the
required vaccines during the visit and some patients
might not be aware of these recommended vaccines.
The rural areas are doing a great job with getting teens vaccinated with the required vaccines, but we need to improve with making sure that teens get all of the recommended vaccines.
In addition, “adolescents don't visit the doctor as frequently as young children,” Stokley said, so it's important during each visit “to take advantage of every opportunity, review the vaccination status of the patient, and recommend and offer vaccines if they're needed.”
“The rural areas are doing a great job with getting teens vaccinated with the required vaccines,” Stokley said, “but we need to improve with making sure that teens get all of the recommended vaccines.”
Success in a Louisiana Clinic
The Louisiana Office of Public Health's Immunization Program reported that Pelican Pediatrics has an age 7 series (DTaP, HepB, VAR, and PCV) rate of 91% and an HPV rate of 50%. According to Louisiana Vaccines for Children, this is higher than the overall Claiborne Parish rate of 78% for the age 7 vaccination series and 44% for the HPV vaccine series.
Brasher said her success rate may be due to her practice's small patient population. “However, I give credit to my staff for being organized and thorough with follow-up,” she added. Her practice's goal is a vaccination rate of 100%.
If patients miss a wellness visit, the staff immediately reschedules the appointment. In addition, Brasher takes time during sick visits to discuss the patient's vaccine record. “If we wait for them to show up for wellness, we miss opportunities,” she said.
Brasher added that her patients respond well to hearing that Brasher vaccinates her own children and that she doesn't receive any extra money or kickbacks from administering vaccines to her patients. She also offers a Vaccine Information Statement and a written handout for parents with questions about vaccines.
Brasher explained that, along with vaccine-hesitant families, she encounters families who are against vaccines. She knows that some providers refuse to see these types of patients. “It took me a while to decide how I felt about taking on these patients because I feel so strongly that children should be vaccinated,” Brasher said. “Recently, however, I came across a family that renewed my interest in taking these patients.”
The mother told Brasher that other providers had refused to see her or shunned her because her child had not received any vaccines. The three-year-old had never attended a wellness visit, and Brasher found out the child was nonverbal. “Had he been seen for a checkup earlier,” Brasher said, “this problem would have been identified earlier and therapy could have been initiated.”
Brasher said that missing appointments in general is a chronic issue in her service area. “If noncompliance with wellness visits could be fixed, then our vaccine rates would go way up.” She reported that school-aged vaccine rates in her service area are good: If parents learn that their children can't attend school without being vaccinated, “they are knocking our doors down to get vaccines.”
Success in Kentucky High Schools
According to the CDC's United States Cancer Statistics, in 2016 Kentucky had the highest age-adjusted rate of new HPV-associated cancers, with 16.6 cases per 100,000 people.
In the academic year 2012-2013, researchers from the University of Kentucky partnered with the Lake Cumberland District Health Department (LCDHD) to implement an HPV vaccination project in two high schools. The team published their findings in a 2015 American Journal of Preventive Medicine article. (The project was funded in part by Merck, but the company had no involvement in the study or publication.)
Even though the HPV vaccine is recommended for 11- or 12-year-olds, LCDHD reached out to the local high schools, since they were eager to collaborate. Dr. Robin Vanderpool, who provided technical assistance to the project, said it's important to gain the schools' buy-in first. She knows of another project in which the team received a small seed grant before talking to the schools; when the schools said no, the team had to return the money. It's important to talk to the teachers as well as the superintendent and principal, she said: “You need the right champions for something like this.”
These schools in south central eastern Kentucky already employed LCDHD nurses, so it was easy for the health department to connect with the schools. In addition, the schools have a built-in health record, so project coordinators could keep track of which students have received which dose of the vaccine series.
I admire the health department director for recognizing [the potential for stigma] and saying we want to make sure every child, no matter their economic status and no matter their insurance status, is offered a chance to participate in this program.
While many students were eligible for Medicaid and therefore free vaccines, project coordinators did not want to single these students out. Instead, they designed the project to reach all students. Vanderpool said, “I admire the health department director for recognizing [the potential for stigma] and saying we want to make sure every child, no matter their economic status and no matter their insurance status, is offered a chance to participate in this program.”
Providing the vaccines onsite “eliminated a lot of the barriers that we think of,” said Vanderpool. “Parents don't have to take off work, take their child out of school, drive them to the pediatrician's office or the doctor's office or the health department, and bring them back to school and check them in.” In addition, students who start the series in the fall can complete it by the end of the school year.
Researchers estimated that about 14% of students in these high schools had completed the HPV vaccination series before this project was implemented. Of the 329 students whose parents consented to have them vaccinated, 288 students completed the HPV vaccination series, a success rate of 88%.
Effective Communication Strategies
In the Kentucky project, coordinators included parental consent forms and information about HPV in students' back-to-school packets. In addition, they used the schools' already existing telephone reminder system to call families when their child's next HPV shot was due. (The parents did not have to be at the school when the child received a vaccine.)
Vanderpool reported some pushback from parents, especially cases where parents had signed many back-to-school forms without fully reading or understanding what they were signing. She advised educating parents through different channels and giving them multiple opportunities to ask questions.
I think often kids are the better educators of parents. Often, kids go home and talk to their parents about what they had learned about health in the classroom.
While project coordinators used newspaper articles, the school website, and other media to raise awareness of this project, Vanderpool said the most effective means of communication was the students themselves. “I think often kids are the better educators of parents. Often, kids go home and talk to their parents about what they had learned about health in the classroom,” she said.
Within the school, students saw their classmates getting out of class to attend a party for those who completed the series; these students also had their names entered in a drawing for gift cards. Students saw these external rewards and became interested in learning more. In addition, because staff and students were talking about the project and raising awareness of HPV, vaccination became a social norm.

In the clinic setting, it's not enough for providers alone to improve their communication skills with families — everyone in the office, from nurses to front-desk staff, should be consistent in their messaging about vaccines.
“If a parent calls because they have to cancel an appointment, they understand why it's critical to reschedule so that they don't go even longer without the recommended vaccine,” Stokley from the CDC said. “Sometimes parents have questions and maybe the front office person is the only person they speak to; at least they'll understand and can convey the message of why it's important to get vaccines. So everyone has a role to help achieve success in the practice.”
The CDC offers resources, like the Getting Your Entire Practice on Board with Vaccinations videos, that providers can share with any staff members who work with patients and their families.
For parents who have questions or concerns, it's important for providers to take the time and really listen to and understand what those parents' particular concerns are and really address those specific concerns.
CDC Health Communication Specialist Ian Branam said, “For parents who have questions or concerns, it's important for providers to take the time and really listen to and understand what those parents' particular concerns are and really address those specific concerns.”
When providers talk with families about the HPV vaccine series, for example, parents may be uncomfortable talking about sexually transmitted infections, so Branam said that providers should focus on the HPV vaccine's ultimate goal: preventing six types of cancer.
Branam also suggested the “bundled recommendation” instead of singling out a particular vaccine and making it seem different from the other shots. For instance, the provider might recommend the Tdap, meningococcal conjugate, and HPV vaccines to the parents of an 11- or 12-year-old patient, rather than recommending the first two and making the HPV vaccine sound optional — and therefore less important. This strategy “places equal emphasis on the importance of all three vaccines,” Branam said.
Branam also emphasized the effectiveness of presumptive language, such as saying, “Your child is due for her vaccines today,” instead of “Are you interested in completing any vaccines today?” One 2017 study of 75 pediatrician visits found that when providers used presumptive language in discussing the HPV vaccine with parents, the parents agreed to vaccinate 73% of the time, compared to a 22% acceptance rate with non-presumptive language.
We know that parents continue to rank healthcare professionals as their most trusted source of vaccine information, so I think that really places healthcare professionals in a unique position to help make that strong recommendation for vaccines and help address any concerns or questions the parents may have.
Cultivating trust and taking the time to listen to and address parents' questions are important in helping patients get vaccinated. “We know that parents continue to rank healthcare professionals as their most trusted source of vaccine information,” Branam said, “so I think that really places healthcare professionals in a unique position to help make that strong recommendation for vaccines and help address any concerns or questions the parents may have.”
Additional Resources
- Vaccination in Rural Communities (CDC) – Offers resources about the HPV and meningococcal vaccines.
- Vaccination Task Force Findings (The Community Guide) – Provides information on interventions like home visits and community education.
- National HPV Vaccination Roundtable action guides – Provides guides for different audiences, including small private practices, providers, and administrative staff.
- #HowIRecommend videos (CDC) – Clinicians share their advice on “Addressing Vaccine Hesitancy or Refusal” and “Making an Effective Recommendation,” among other topics.

