Jun 16, 2021
Still Stealing Rural America's Breath: An Update on Chronic Obstructive Pulmonary Disease
 In January 2017, the Centers for
Disease Control and Prevention (CDC) released reports
that not only revealed the five leading causes of
death in the U.S. but also spotlighted the rural-urban
disparity of those medical conditions. Heart disease,
stroke, cancer, and unintentional injuries were on this
list, along with chronic lower respiratory diseases. This
latter category included chronic obstructive pulmonary
disease, or COPD. Of those categories, COPD was a
condition of much concern. In a 2017 Rural
Monitor interview, patient advocate and 2016-2018
COPD
Foundation president Grace Anne Dorney Koppel
articulated why COPD was of importance to rural America.
In January 2017, the Centers for
Disease Control and Prevention (CDC) released reports
that not only revealed the five leading causes of
death in the U.S. but also spotlighted the rural-urban
disparity of those medical conditions. Heart disease,
stroke, cancer, and unintentional injuries were on this
list, along with chronic lower respiratory diseases. This
latter category included chronic obstructive pulmonary
disease, or COPD. Of those categories, COPD was a
condition of much concern. In a 2017 Rural
Monitor interview, patient advocate and 2016-2018
COPD
Foundation president Grace Anne Dorney Koppel
articulated why COPD was of importance to rural America.
“Over the past 15 years, there is this growing divide between rural and metropolitan America, especially for the five leading rural causes of excess deaths,” Koppel had said. “Despite this rural divide, rural death rate trends for cancer, heart disease, diabetes, all are going in the right direction. Except for one chronic disease. That exception is COPD. This must change.”
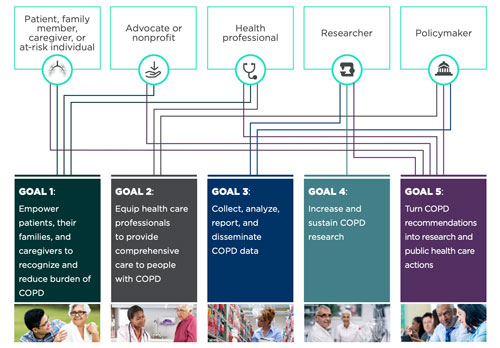
Fast forward to 2021: Though the morbidity and mortality data haven't changed much yet, experts point out that the action to drive change started in 2017 with the National Heart, Lung, and Blood Institute's (NHLBI) launch of the COPD National Action Plan. Created in partnership with the CDC and the COPD stakeholder community, it was an original response to the 2012 Senate Appropriation Committee request to address the nation's growing COPD problem. The plan includes five goals and identifies five major stakeholder groups.
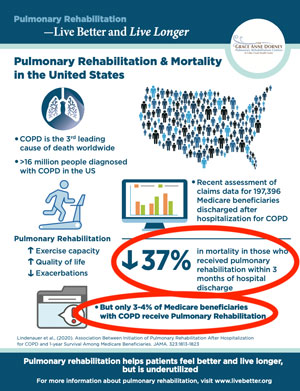
Now five years into the plan, researchers, advocates, and other professionals talk about rural COPD issues and what's still needed to address the condition that is stealing rural America's breath, including the need for pulmonary rehabilitation, long known to improve quality of life — with new research proving it decreases death rates.
What Do We Know About COPD?
- Rising death rate compared to stabilized/decreasing death rates of the top 5 leading causes of death
- 4th leading cause of death, behind heart disease, cancer, and unintentional injuries (including opioid overdoses)
- Affects non-smokers as well as smokers
- Escalating disease-related cost: 2010 estimation of $32 billion to nearly $50 billion in 2020
What Do We Know About COPD in Rural America?
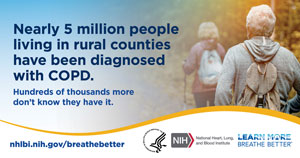
- 5 million rural Americans have COPD
- Hundreds of thousands more don't know they have it
-
Compared to urban/large metro center residents with
COPD:
- Almost twice as many rural Americans have COPD
- Almost twice as many rural Americans die from COPD
- In 2015, rural Medicare patients experienced 27% more hospitalizations and 71% more deaths from COPD than urban patients
- For rural residents living in poverty, COPD prevalence again increases
COPD National Action Plan Five Years Later: Where the Rural Research Action Is
Dr. Antonello Punturieri, an NHLBI program director and participant at the Action Plan's design table, said he's been pleased with research activities that are moving forward because of the plan.

“There has been a strong response from government and non-government partners around the issues related to COPD,” Punturieri said. “These responses have shed light on many issues ranging from information about who is affected, to where these persons live, to how they get their care for COPD — as well as exploring the links to the other diseases or comorbidities that invariably are seen in patients with COPD.”
Punturieri said the rural response has been significant. He commented on the willingness of the rural community to engage in the efforts around COPD.
“The rural engagement has been remarkable,” he said. “From the involvement of rural associations and their partners to a specific collection of rural COPD data by the CDC, there now seems to be a shift with more researchers contemplating proposals exclusively targeting COPD in rural settings.”
Punturieri said he also sees that shift in COPD research represented by a definite increase in proposals aimed at exploring the ruralness of the disease, its causes, and treatments. Additionally, through the work of the National Institutes of Health (NIH) Rural Health Interest Group, Punturieri pointed out that the agency's COPD research activities are being linked with research around other chronic diseases. He explained that this is intentional and has the potential to exponentially raise the research impact since COPD is usually not a stand-alone condition in any patient in any location.
He also emphasized that research is complicated in rural populations due to industrial, agricultural, and livestock exposures, like air particulates linked to raising cattle and hogs.
“Researchers have to shift their thinking and their investigative approach because it's much more complex,” he said. “They have to consider how they can exclude X, exclude Y. They have to think in terms of how the disease is triggered and how they can study avoidance interventions, which are so critical when trying to determine what really triggers the condition.”
COPD and NHLBI Rural-Focused Activities
Punturieri shared some specific NHLBI activities linked to COPD:
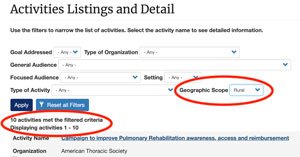
- COPD National Action Plan Community Action Tool: Launched in 2021, this new system is available for stakeholders to track progress toward the Plan's goals and objectives and includes the ability to filter by rural geographic scope. Rural organizations can enter their activities related to the Action Plan's goals and objectives.
- Multiple research projects that include rural practice sites, such as the CAPTURE study, exploring a simple diagnostic tool to identify people with a high likelihood of having COPD
- Other currently funded research includes projects
studying:
- Increasing adherence to pulmonary rehabilitation after COPD-related hospitalizations
- Evaluating organic dust within livestock production buildings as a risk factor for chronic bronchitis development
Past NIH/NHLBI COPD-Focused Public Meetings
2018: COPD & Rural Health: A Dialogue on the National Action Plan
2019: COPD National Action Plan: Tracking Our Progress, including rural-specific reports
Understanding Rural Policy Issues Around COPD
As Punturieri suggested, closing in on the rural-urban disparity associated with COPD and chronic respiratory diseases has been boosted by engagement of diverse rural COPD interest groups. Using their collective voice, 25 federal and state agency leaders, researchers, advocacy groups, and individuals spoke out in a 2019 paper in the Journal of Rural Health, COPD and Rural Health: A Dialogue on the National Action Plan. Working through the five goals, the authors concluded: “COPD is a common, underdiagnosed, undertreated, and devastating chronic lung disease prevalently affecting underserved communities such as those of rural America. A concerted effort from all interested parties will make a difference in the lives of people and families affected by COPD and the communities in which they live.”
COPD and Rural-focused Policy Issues
The Federal Office of Rural Health Policy (FORHP) has been involved with rural COPD-focused efforts along with the National Advisory Committee on Rural Health & Human Services. In its 2018 letter to Alex Azar, then Secretary of Health & Human Services, the committee included its policy brief, noting the committee had made a North Carolina site visit to one of the many rural pulmonary rehabilitation centers supported by the Dorney-Koppel Foundation. Three policy recommendations were provided to the Secretary:
- Establish a national rural primary care provider COPD education campaign emphasizing screening and treatment.
- Prior to any subsequent outpatient prospective payment rate changes, obtain expert consultation to refine the definition of pulmonary rehabilitation services and Medicare cost reports to adequately set reimbursement rates.
- Expand pulmonary rehabilitation direct supervision requirements to include physician assistants, nurse practitioners, and other primary care providers under general supervision of a physician.
Philanthropy Making a Difference for Rural COPD
A strong voice for rural people with COPD is Grace Anne Dorney Koppel. Dorney Koppel is past president of the COPD Foundation and current president of the Dorney-Koppel Foundation. The foundation supports 9 pulmonary rehabilitation (PR) centers in rural and urban areas with a high prevalence of COPD. The recipient of the 2020 National Rural Health Association's Outstanding Rural Champion Award, Dorney Koppel was also at the Action Plan design table. Reflecting over the past five years, she commented on gains around the condition, the impact of COVID on the Plan's goals, and the remaining gaps around the needs of COPD patients.

“When the COPD National Action Plan was released, the CDC's information on the five leading causes of death had already brought recognition of the health disparities between urban and rural locations,” Dorney Koppel said. “Those disparities came as a surprise to many people. Though the disparities were great, rural death rates for heart disease, stroke, and diabetes were at least stabilizing or improving. However, in contrast, it was absolutely chilling to see that COPD was not following that trend. In those moments came the recognition that the disparity with COPD could no longer be ignored.”
Dorney Koppel said that the COVID-19 public health emergency (PHE) has impacted the Plan's momentum in multiple ways. First, she said she believes it has elevated public understanding of the daily struggle for breath that many people with COPD live with much of the time.
“Breathing is a commodity that is essential for life,” she said. “The dynamic at play with COVID is that difficulty breathing is now better understood because it is one of the most profound problems for those who acquire the infection. Because of this comparison, more people can now understand the breathing struggles many COPD patients have.”
Second, she emphasized that much of the growing collaborative energy between rural researchers, advocacy groups, clinicians, national professional organizations, and federal agencies halted when energies had to be redirected to the PHE. She checked off the items that now seem perpetually present on the COPD to-do list: increase federally funded research from current levels of pennies-per-patient; create a permanent, disease-specific surveillance database; identify the millions of Americans who have COPD yet remain undiagnosed; develop new medications; and launch a primary care provider education campaign to improve identification and treatment of COPD as well as to increase referral to pulmonary rehabilitation.
Lastly, she said COVID has had a marked negative impact on the most beneficial treatment for COPD: pulmonary rehabilitation (PR).
“COVID distancing has led to a pause in so many of the few rural pulmonary rehab centers,” she said, noting the tremendous positive impact of PR in her own life as a person with severe COPD. “Because of current reimbursement rules, some will never reopen. On the other hand, NIH and other funders are now supporting studies and clinical trials that focus on delivering the essential elements of PR via telehealth. These remote PR programs can have a profound impact on COPD treatment since many more rural COPD patients may be able to attend PR in their own homes.”
Along with addressing COVID's negative impact, Dorney Koppel also pointed out how reimbursement has long impacted existing PR programs and limited new program growth. However, she said she remains hopeful that the reimbursement challenge for PR will be reconsidered in light of new research that shows a decreased mortality rate for those who enter a PR program soon after a COPD-related hospital discharge. She shared that this finding has provided the impetus for a public awareness campaign to promote the benefits of PR.
“A landmark paper just published in 2020 reveals that pulmonary rehabilitation can decrease mortality by almost 40% if PR is begun within 90 days of hospital discharge for a COPD exacerbation,” Dorney Koppel said. “Forty percent! We've long known that PR improves quality of life, but this new information on mortality could be a turning point, especially for reimbursement arguments. We deserve this. We have no new drugs. The best therapy that we have now that can enable us to live better and live longer is pulmonary rehab. This is a very powerful message for rural COPD patients since COPD is twice as prevalent in rural than in urban America.”
COPDSOS.org: New Public Awareness Campaign to Find the Missing Millions with COPD
Thirty million Americans have COPD, but half of these people don't know it. As with many chronic diseases, early diagnosis and treatment can have great impact on the health and well-being of people unaware that they have COPD. For those yet undiagnosed, they are even more vulnerable to poorer outcomes if they become ill with COVID-19.
Partnering with the COPD Foundation, the American Respiratory Care Foundation (ARCF), and other foundations and funders, the Dorney-Koppel Foundation has a mission to find the “missing millions” with undiagnosed COPD. The organizations are planning a countrywide public awareness campaign. Its web-based platform, COPDSOS.org, also includes materials such as patient testimonials and a COPD risk assessment questionnaire.
More On Pulmonary Rehabilitation from Program Leaders

Gayla Oakley from rural Nebraska and Aimee Kizziar, having grown up in rural Minnesota but now located in urban California, echo Dorney Koppel's concerns. Their leadership roles at the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) allow them a national perspective on the multiple issues associated with PR, ranging from start-up challenges experienced by new rural PR programs and on through the needs of additional issues as addressed by one of their colleagues in Pulmonary Rehabilitation Reimbursement – Time for All of Us to Be Part of the Solution.
Kizziar shared that AACVPR has joined 18 other organizations — including the Dorney-Koppel Foundation — to provide a singular endorsement for PR.

“I feel like the tides are changing,” Kizziar said. “With the recent paper demonstrating a 40% decrease in the risk of death for patients participating in post-hospitalization pulmonary rehab and these societies and organizations uniformly endorsing pulmonary rehabilitation, we are better positioned to get this treatment offered in more locations to more people with the condition.”
Rural Nebraska's Oakley, also director of cardiac and pulmonary rehab at her organization, said it's important that unanimous support for PR be used to gain parity and stature in rural America.
“Despite the fact that they are in a different setting, smaller rural programs in Critical Access Hospitals can provide the same rehab service as larger urban programs,” she said. “The key is to maximize your resources.”
More about PR in Rural America
Oakley's AACVPR role often connects her with peers in small and rural organizations interested in quality improvement or starting new programs. Oakley said that AACVPR has numerous resources for rural areas and also suggested that, depending on location, the 34 state and 4 regional affiliates are an additional professional network that can understand the specific local needs of current programs or plans for new PR programs.
“It's important to understand that all rural is not equal,” she said. “The problems and challenges that we face here in Nebraska will not be the same as rural Mississippi or any other state. The state and regional affiliates understand those differences.”
Oakley and Kizziar shared that an important part of their
job is educating medical professionals and their peers
about PR benefits. For example, Kizziar shared that she
frequently hears from patients that they have been told
by their providers they should not exercise
— or have been told that, now that they need
oxygen, they need to conserve as much energy as possible.
More in This Series
Despite start-up challenges, several rural organizations are taking the leap and starting programs. Learn about their work and more general information about pulmonary rehabilitation in the second of this 2-part Rural Monitor rural COPD series, Pulmonary Rehabilitation Programs: Benefiting Rural Individuals, Benefiting Rural Population Health.
“Patients that finally get to pulmonary rehab
are just so amazed about how much their lives change with
just the breathing retraining,” Kizziar said.
“With the exercise part of the program, their
endurance and energy increase dramatically. You can't
imagine how they feel when they can take walks with their
significant others, hold grandchildren, or advance from a
completely sedentary lifestyle to being able to even just
take out the garbage. This makes provider education so
important in order to dispel the myth about exercise and
other issues for these patients.”
Oakley also shared the surprises around the myths and realities of PR.
“For as long as pulmonary rehabilitation has been in existence — and our program at our Critical Access Hospital started in 1989 — I'm still surprised when people comment about my job as one of going to work and just supervising exercise,” Oakely said. “Those comments allow me to provide some serious education about PR benefits. For example, I talk about the extensive education for patients about their chronic lung disease and self-management and how individual action plans are created. We give patients breathing techniques that match their needs. We teach them about their medications and how to use their inhalers so that the medication in the inhaler can actually work for them.
“In addition to that information, now it's important that we share the recent data that there's almost a 40% decrease in risk of death if PR starts after a hospitalization for COPD. Pulmonary rehab is incredibly worthwhile for any patient with limits from chronic lung disease. With PR, they do better, they feel better, and are incredibly appreciative of the way the program changes their life. That's why it's so easy for me to get up every morning and care for these patients.”
Resources
Centers for Disease Control and
Prevention
Chronic
Obstructive Pulmonary Disease
National Heart, Lung, and Blood
Institute
Chronic
Obstructive Pulmonary Disease
Learn
More Breathe Better program
Rural Health Information Hub
Other Rural Monitor stories:
- Diagnosing the Rural COPD Patient: Ask About Symptoms, Use Spirometry
- Office-Based Spirometry: Key to Diagnosing Rural COPD Patients
- Pulmonary Health in Rural America: Cause and Impact of Work-Related Lung Diseases
Toolkit: Rural Chronic Obstructive Pulmonary Disease Toolkit
Video: The Challenges of Chronic Disease in Rural Areas: Chronic Obstructive Pulmonary Disease (COPD)

