The Health-able Communities Program
- Need: Expand healthcare access for the more remote residents of 3 frontier counties in north central Idaho.
- Intervention: Consortium of healthcare providers and community agencies used a hybrid Community Health Worker model to augment traditional healthcare delivery services in order to offer a diverse set of healthcare offerings to frontier area residents.
- Results: Increased healthcare access, especially for cancer and chronic disease screening, along with providing education on a diverse array of health topics.
Evidence-level
Promising (About evidence-level criteria)Description
In a region some consider one of the Pacific Northwest's most geographically isolated areas, 28,000 people reside in frontier Idaho's Clearwater, Idaho, and Lewis counties. Here, healthcare access is limited not just by distance and transportation barriers, but by the limited number of medical providers practicing in the area. These factors likely contribute to startling county-level statistics associated with suicide, cancer, and chronic diseases such as diabetes, hypertension, and obesity. St. Mary's Hospital, a Critical Access Hospital (CAH) in Cottonwood, Idaho, and its associated facilities led a consortium of 9 partners in a project offering health education and disease screening for residents in these counties.
The project, the Health-Able Communities Program, leveraged a specially-trained professional force of Community Health Workers (CHWs). The consortium leaders pooled different components of several well-known evidence-based CHW models to create a hybrid CHW role for addressing the area's specific medical needs and related needs linked to the social determinants of health.
Eleven CHWs performed disease screenings, provided general health and wellness education, and led chronic disease self-management programs. Their modified roles allowed them to receive referrals from medical providers and community members in order to offer assistance to residents in even the most remote locations. CHWs were overseen by physicians and nurses. They were also part of some medical home teams.
In addition to the St. Mary's team, the project's consortium members included:
- 2 additional CAHs – Clearwater Valley Hospital and Clinics, Syringa Hospital
- 2 health services agencies – Grangeville's and Clearwater's Human Needs Councils
- Public health department – Idaho North Central Health District
- Indian Health Service clinic – Nimiipuu Health
- Free urban clinic – Snake River Community Clinic
- Tertiary care center – St. Alphonsus Regional Medical Center
St. Alphonsus Regional Medical Center provided education on mental health topics. The councils provided other resources and the public health department assisted with CHW training.
The project's data tracking was accomplished with REDCap, a system that allowed surveys as well as some data analysis. All partners worked together to develop a 5-year strategic plan for program sustainability.
Support for this project came from the Federal Office of Rural Health Policy's 2015-2018 Rural Health Care Services Outreach Program funding.

Services offered
CHW activities:
- Assisted in the creation of walking trails, community gardens, and community education centers
- Organized community screening events and:
- Performed hemoglobin A1C testing for diabetes screening and evaluation
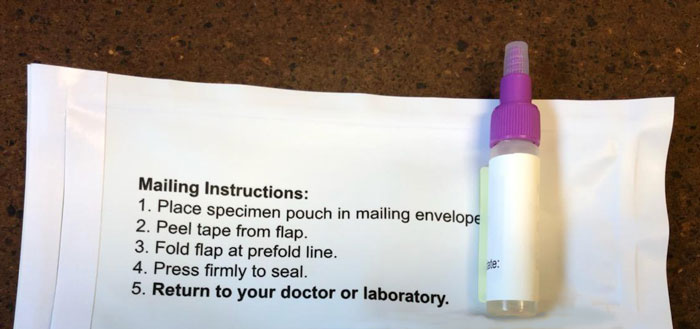
- Provided FIT colorectal cancer screening tests and for any positive result, assisted willing patients with follow-up testing
- Measured body mass index (BMI) and blood pressure
- Conducted depression screenings
- Taught Chronic Disease Self-Management Program (CDSMP) classes which were open to the public
- Made remote home visits
- Assisted with medication delivery in more remote areas
Results
- During the 3-year grant cycle, nearly 3,000 people were evaluated at over 100 events to reach approximately 10% of the population in the tri-county area
- Performed over 750 FIT tests, an activity which
screened approximately 7% of the population eligible for
colorectal cancer screening
- 49 participants with positive FIT tests were offered assistance with follow-up arrangements
- Increased access to healthcare
- Increased referrals to social service agencies
- Multiple positive—and some life-saving—anecdotal patient care stories related to CHW activities
- Overall program success led to ongoing discussions with government insurance payers (Idaho Medicaid) around designating CHW interventions as billable services
Other qualitative results:
- CHW role validated in 3 major areas:
- Served as additional health education providers
- Increased community awareness prevention/wellness activities
- Increased healthcare system access due to the CHW role as trained outreach health professional providers
- Multiple positive—and some life-saving—anecdotal patient care stories related to CHW activities
- Overall program success led to ongoing discussions with government insurance payers (Idaho Medicaid) around designating CHW interventions as billable services
Models used to develop hybrid CHW for Health-able Communities:
- Sinai Health System's (now included in the American Hospital Association's information) Best Practice Guidelines for Implementing and Evaluating Community Health Worker Programs in Health Care Settings.
- Centers for Disease Control and Prevention's Addressing Chronic Disease through Community Health Workers.
- Federal Office of Rural Health Policy's Community Health Workers Evidence-based Models Toolbox, current version available online as the Community Health Workers Toolkit.
Consortium members have been invited as presenters to multiple state and national gatherings and conferences.

Challenges
- CHW recruitment/retention and need for continual recruitment
- Unanticipated costs for:
- Mobile hemoglobin A1C monitors that required more expensive reagents/testing kits than hospital stationary machines
- High number of individuals qualifying for screening intervention
- Hemoglobin A1C test performance time interval
- This test performance time necessitated additional CHW personnel at screening events in order to keep waiting participants engaged
- Unanticipated travel expenses required to cover geographic footprint of service area
- Tracking extensive data categories associated with project activities
Replication
- Inclusive recruitment of an area's healthcare organizations and related community agencies will provide the broadest outreach and services to meet a specific region's needs.
- Identify the correct data-tracking system for CHW work, for example, REDCap.
- Develop team leadership skills for CHWs.

Contact Information
Shari Kuther, RN, Director of Population HealthSt. Mary's Clearwater Valley Hospital and Clinics
208.962.2473
shari.kuther@smh-cvhc.org
Topics
Access
Cancer
Cardiovascular disease
Chronic disease management
Community health workers
Diabetes
Frontier and remote areas
Health disparities
Health screening
Wellness, health promotion, and disease prevention
States served
Idaho
Date added
March 28, 2019
Date updated or reviewed
April 28, 2021
Suggested citation: Rural Health Information Hub, 2021. The Health-able Communities Program [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1054 [Accessed 26 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
