Vermont Hub-and-Spoke Model of Care for Opioid Use Disorder
- Need: Increase access to medication-assisted treatment for opioid use disorder in rural Vermont.
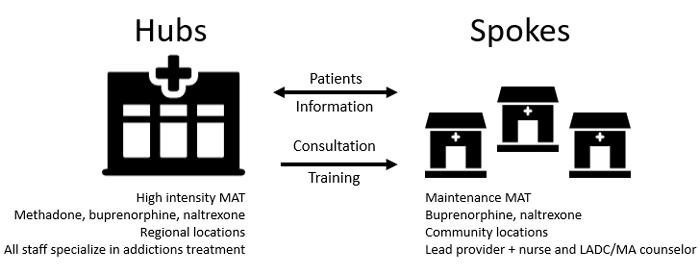
- Intervention: Statewide hub-and-spoke treatment access system.
- Results: Increased treatment capacity and care coordination.
Evidence-level
Effective (About evidence-level criteria)Description
With over 9,000 square miles, Vermont has a significant rural population. Eight of its 14 hospitals are designated as Critical Access Hospitals. Though in the past Vermont was a leader for a number of waivered providers for office-based opioid treatment (OBOT) of opioid use disorder (OUD), providers were treating limited numbers of patients because of treatment-related challenges and lack of behavioral health partners.
Additional treatment barriers to medication-assisted treatment (MAT) for OUD were provider concerns for reimbursement as well as drug diversion problems, the transfer of one individual's legally prescribed controlled substance to another for illicit use. To mitigate these issues for rural areas as well as for the entire state, the Care Alliance for Opioid Addictions Initiative (2012-2016) was created by addiction medicine specialists and public health leaders. This approach is unique in linking OBOT and hub-based opioid treatment programs (OTP). In 2017, Vermont had the highest capacity in the U.S. for treating OUD.
Central to the project was replicating chronic disease management principles, similar to congestive heart failure clinics staffed by cardiologists or HIV clinics with infectious disease specialists. In the Care Alliance model, addiction medicine specialists and specialty clinics were matched to initial treatment or relapse management of OUD using a coordinated hub-and-spoke treatment model that adapted a continuum of care model embracing collaboration and integration efforts.
Also built into the model was a unique bidirectional transfer process: the hub could transfer care to the spoke, and vice versa. Patients were transferred into the hub for assessment and initial medication induction and medication stabilization. Once stable, patient care was transferred to the spoke. If the patient relapsed/destabilized, the spoke transfers the patient back to the hub.
A learning collaborative was a key element to the dissemination and implementation of this robust, comprehensive, statewide program.

The Care Alliance designated 5 geographic hub clinic areas where outpatient methadone treatment programs were given additional prescriptive authority for buprenorphine, an opioid blocking drug. Coordinated transfers between the hub and spoke was an intentional goal. Specifically, once patients were stabilized, they were transferred from the OTP to their primary care provider or a medical home for further OBOT.
Funding for the treatment leveraged reimbursement through aspects of the Affordable Care Act's Home Health Services' Community Health Teams. The National Institutes of Health and the National Institute of General Medicine Science also provided grant support for this project.
Services offered
Hub:
- Specialty clinics with board-certified addiction
specialists:
- Perform comprehensive physical and mental health evaluations
- Provide treatment with buprenorphine or methadone, depending on patient assessment
- Referrals to the hub originate from hospitals, emergency rooms, residential treatment programs, correctional facilities, and community mental health programs
Spoke:
- Spoke-located Care Alliance MAT
team:
- The Vermont Chronic Care Initiative provides 1 full time RN and 1 master's-level licensed behavioral health provider/100 treated patients providing clinical, logistical, and administrative duties that increased spoke provider prescribing efforts
- Provides interested physicians with waiver-training information
- Waivered providers are provided with on-going support when needed
Diversion Prevention:
- At both hub and spoke locations, patient medication dosing is observed to prevent diversion.
Incarcerated population:
- In 2018, No. 176 (S.166) was passed mandating provision of MAT for inmates. At time of release, most clients had immediate access to hub or spoke care.
Results
Data from early implementation:
Pre-implementation MAT wait times varied within the state. However, during 3-year implementation phase:
- 2 regions eliminated treatment waiting lists
- 2 regions nearly eliminated treatment lists
- 1 region decreased waiting list from 6 months to 2 months
Waivered physician increased from 2012-2016, from a total of 173 to 283 providers. Additionally, there was a 50% increase in providers caring for more than 10 patients. By Sept 2015, 23% of spoke providers were caring for more than 30 patients and 10% caring for more than 50 patients.
Successes of early implementation that led to the program's ongoing success and sustainability were:
- In 2019, an estimated 15,000-20,000 people were
determined to possibly benefit from MAT, total Vermonters
on MAT number nearly 8,600 which corresponds to 1.7% of
the adult population. Numbers remain similar for 2020.
- In 2018, overdose deaths in Chittenden County, Vermont's largest county, dropped by 50% likely due to expanded low barrier options at the Medical Center Emergency Department and the Howard Center needle exchange program providing same day initiation of buprenorphine.
- No clients waiting for hub services
- June 2018 through May 2019: 23% increase in number of buprenorphine-waivered prescribers
- Between the first quarter of 2016 and first quarter 2020, the state has seen a 46% decrease of opioid prescriptions as measured in MME — morphine milligram equivalents — a way to standardize opioid prescriptions.
- Incarcerated population: With Act 176 passed in 2018, by Feb 2019, 16% of all inmates were on MAT and by November 47% of the nearly 1500 previously incarcerated individuals were receiving MAT.
Note: Monthly updates are available through the state department of health.
For more program details:
Rawson, R., Cousins, S., McCann, M., Pearce, R., Van Donsel, A.. (2019) Assessment of medication for opioid use disorder as delivered within the Vermont hub and spoke system. Journal of Substance Abuse Treatment; 97:84-90. [Abstract.]
Brooklyn, J.R., Sigmon, S.C. (2017). Vermont Hub-and-Spoke Model of Care For Opioid Use Disorder: Development, Implementation, and Impact. Journal of Addiction Medicine; 11(4):286–292.
Vermont Hub-and-Spoke Model of Care for Opioid Use Disorders: An Evaluation. Richard A. Rawson. Vermont Center on Behavior & Health, The University of Vermont. December 2017.
Collaborative Models for Medication-assisted Treatment Key Elements of Vermont's Hub-and-Spoke System. Medicaid Innovation Accelerator Program, April 2019.
Vermont Results First Inventory and Benefit-Cost Analysis. Crime Research Group, December 2017.
Challenges
- Staffing shortages
- Data collection across treatment network
Replication
To replicate this project's success in other states or regions:
- Involve passionate physician leaders
- Understand that spoke MAT teams are integral to achieving success
- Provide education for policy makers:
- Chronic disease aspects of OUD
- MAT waiver training is not equal to addiction medicine certification
- Use Learning Collaborative to promote common language central to achieving project goals
- Entertain Medicaid expansion as necessary for overall success
- Partnering with a state health department that's committed to providing comprehensive MAT access
Contact Information
John R. Brooklyn M.D., Clinical Assistant ProfessorDepartment of Psychiatry, The University of Vermont
johnr.brooklyn@gmail.com
Topics
Access
Illicit drug use
Prescription drug misuse
Service delivery models
Substance use and misuse
States served
Vermont
Date added
June 13, 2018
Date updated or reviewed
August 7, 2020
Suggested citation: Rural Health Information Hub, 2020. Vermont Hub-and-Spoke Model of Care for Opioid Use Disorder [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1015 [Accessed 26 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
